Online CPR Certification Blog
What are the Disadvantages of CPR?
Date: March 11th, 2024
CPR, or cardiopulmonary resuscitation, is often lauded as the life-saving act that comes to our mind when someone’s heart stops. Movies and TV shows have romanticized its effectiveness, and while it indeed has saved countless lives, it’s essential to understand its complete spectrum. So,
let’s embark on this journey of understanding CPR beyond the surface.
Physical Risks to the Recipient
The act of performing CPR involves a considerable amount of force. Such force, while vital, can sometimes lead to unintended consequences.
Fractures
Our skeletal structure isn’t always prepared for the intense pressure applied during CPR:
- Ribs and sternum: These bones, especially in older individuals, can break. Brittle bones can easily fracture, causing internal complications.
Lung Complications
Saving a life isn’t without risks. The lungs, being close to the sternum, are particularly vulnerable:
- Punctured Lung: It’s a frightening scenario but a possibility when ribs break and puncture the lung.
- Aspiration Pneumonia: As CPR is performed, especially without an airway device, stomach contents might find their way into the lungs, leading to a dangerous infection.
Brain Damage
Time is of the essence in CPR. The brain’s need for oxygen is paramount:
- Oxygen Deprivation: Brain cells start dying within minutes without oxygen, leading to potential long-term damage.
Effectiveness and Outcomes
Let’s be real; CPR doesn’t always have the desired outcome.
Success Rates
- Reality Check: CPR, when performed outside of hospital settings, often has a lower success rate, sometimes as low as 2-11%. It’s a sobering statistic but crucial to know.
Temporary Solution
- A Battle Half-won: Even if CPR manages to restart the heart, the underlying medical condition remains. This means the patient still requires urgent medical care.
Life Post-CPR
- Aftermath: Surviving cardiac arrest doesn’t always mean going back to normal. Many patients face neurological issues or physical disabilities.
- Rehabilitation: Often, an extended period of medical care and rehab follows, demanding resilience from both patients and their families.
Emotional and Psychological Impact
The ripple effect of CPR goes beyond the physical. It touches the mind, soul, and spirit.
On the Recipient
Waking up after a near-death experience can be overwhelming:
- Mental Struggles: Fear of recurrence, anxiety, and even symptoms of post-traumatic stress can emerge.
On Bystanders and Family
Watching a loved one in such a critical state is a memory that often lingers:
- Distress: Witnessing CPR can be traumatic, raising questions about mortality and vulnerability.
- Second-Guessing: Doubts about the decisions made during the emergency can haunt family members.
Risks to the Rescuer
Performing CPR is no walk in the park. It demands physical strength, mental clarity, and a great deal of courage.
Physical Strain
- Exertion: The act can be tiring, potentially causing muscle strain or injury to the rescuer, especially if performed for an extended period.
Infection Risk
- Safety First: Rescuers might be exposed to bodily fluids, which, without protective barriers, could lead to the transmission of diseases.
Emotional Burden
- Heavy Heart: Not succeeding in reviving someone can leave emotional scars, leading to feelings of guilt and inadequacy.
Legal and Ethical Concerns
The decision to perform CPR isn’t always black and white, and sometimes, the gray areas can be tricky to navigate.
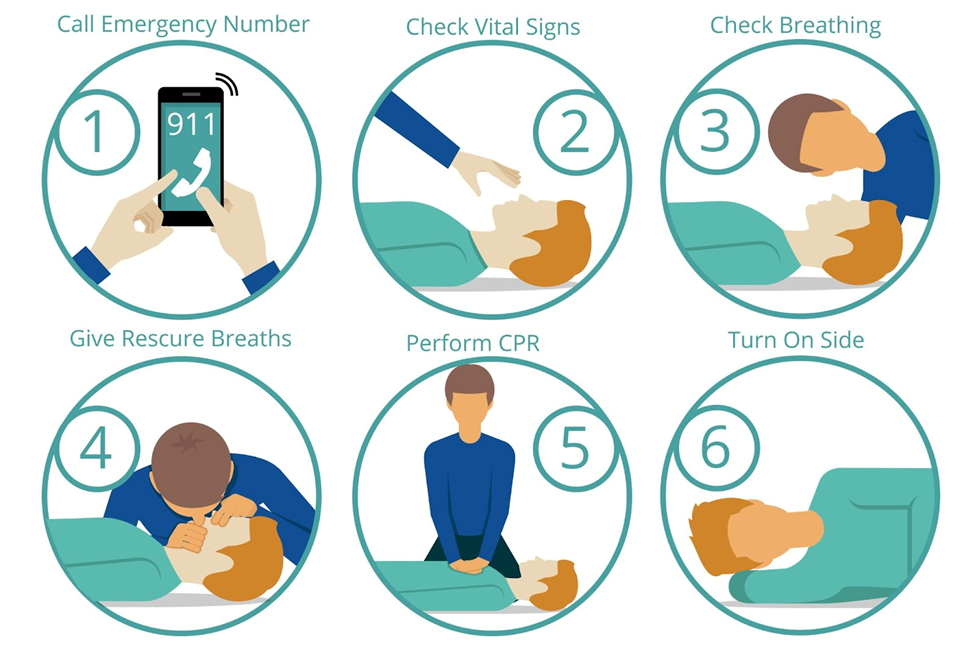
Alt Tag: an illustration showing the cardiopulmonary resuscitation process
Author credit: By Rama – Own work, CC BY-SA 2.0 fr, https://commons.wikimedia.org/w/index.php?curid=3632271
Informed Consent
- DNR Dilemma: A Do Not Resuscitate order means a patient doesn’t want to be resuscitated. But in emergencies, especially outside a hospital, these may be unknown or overlooked.
Liability
- Legal Consequences: Despite the best intentions, if CPR is performed incorrectly, it might result in legal actions.
Moral Dilemmas
- Ethical Questions: Especially in cases of terminally ill patients, the decision to perform CPR can raise questions about the quality of life versus the act of saving life.
Advanced Directives and Their Importance in Medical Decisions
In the world of medical emergencies and critical care, CPR is a topic that’s often discussed. Yet, what’s equally vital, but less frequently broached, is the concept of Advanced Directives. Let’s dive into why this topic matters so much, especially when discussing CPR.
What Are Advanced Directives?
Advanced Directives are legal documents that specify what actions should be taken for a person’s health if they are no longer able to make decisions for themselves because of illness or incapacity.
They come into play in situations like the end of life care, long-term illnesses, or severe medical emergencies.
Types of Advanced Directives
- Living Will: Describes the kinds of medical treatments you would or wouldn’t want in specific situations.
- Durable Power of Attorney for Health Care (or Health Care Proxy): You appoint someone to make medical decisions for you if you can’t speak for yourself.
- Do Not Resuscitate (DNR) Orders: As we touched on earlier, this specifies that you don’t want CPR if your heart stops or if you stop breathing.
Why Are They Important?
- Clarity in Emergencies: In intense situations, emotions can run high. Advanced Directives provide a clear roadmap of the patient’s wishes.
- Avoiding Unnecessary Procedures: If a patient doesn’t want certain treatments, like CPR, it prevents potential complications or prolonged suffering.
- Empowerment: It ensures that individuals have a say in their care, even when they can’t voice their opinions.
- Easing the Burden: For loved ones, making critical decisions can be taxing. Advanced Directives take the guesswork out and reduce potential conflicts or feelings of guilt.
CPR and Advanced Directives – The Connection
CPR, being a life-saving procedure, can sometimes work against a patient’s wishes if they desire a natural end or if they’re suffering from a terminal illness.
Here’s where Advanced Directives step in. They act as a guideline, ensuring that medical professionals and caregivers adhere to the patient’s wishes, even in the frenzy of emergencies
FAQs
How often does CPR result in broken ribs?
Surprisingly often, especially in elderly patients. Up to 30% of CPR recipients might experience rib fractures.
What is a DNR order?
A DNR is a legal directive. Those with a DNR order wish NOT to be resuscitated in emergency situations.
Can someone fully recover after receiving CPR?
Some do, but recovery depends on factors like the duration of oxygen deprivation and the initial cause of the cardiac arrest.
Should I act or wait if I’m unsure about performing CPR?
In emergencies, it’s generally better to act. Even if not perfect, your actions might give the person a fighting chance.
Am I protected legally if I perform CPR?
Many places have “Good Samaritan” laws protecting those assisting in emergencies, but it’s always wise to be familiar with local regulations.
The Bottom Line
CPR is undeniably a beacon of hope during life-threatening situations. However, with hope comes responsibility, understanding, and awareness of its broader implications.
By comprehending its entire scope, we can make informed choices when the time calls.
