Online CPR Certification Blog
Why You Might Have Fluid Around Your Heart – And What To Do About It
Date: December 27th, 2022
Fluid Around Your Heart: What Causes It?
One of the most common reasons people visit their cardiologist is because they have fluid around their heart, also known as pericardial effusion.
What exactly does this mean? And why does it happen? Is it something that needs immediate action?
Let’s look at what could cause fluid around your heart and what to do to relieve your symptoms and get back to living your life.
Understanding the Pericardium
The pericardium is the place where this fluid accumulates. It is made up of two layers:
- an outer layer, which contains elastic fibers called elastin and collagen fibers;
- an inner layer, which includes cardiac muscle cells called myocardium.
The pericardium is a protective barrier between your body’s inner organs and the exterior environment. The pericardium also serves to maintain blood pressure by restricting blood flow to some heart regions to keep pressure levels stable.
When pericardial effusion occurs due to inflammation or infection of the heart’s lining, fluid builds up around your heart’s inner chambers (the atria). This fluid buildup can cause several symptoms, including shortness of breath, chest pain, and fatigue.
Causes of Pericardial Effusion or Fluid Around Your Heart
Pericardial effusion is the medical term for when there’s an abnormal amount of fluid around the heart. Although it’s usually benign, in some cases, it can be a sign of a more severe condition. Fluid can accumulate for a variety of reasons, including:
- Injury to the heart or pericardium (the sac that surrounds the heart)
- Malignancy (cancer) involving the heart
- Congestive heart failure
- Pleural effusion (fluid around your lungs)
- Cardiac tamponade (a type of pericardial effusion caused by blood filling up within the chest cavity, compressing other organs and causing shortness of breath)
- Fluid accumulation due to injury
Noncancerous conditions like idiopathic pulmonary fibrosis, sarcoidosis, vasculitis, Kawasaki disease, and severe asthma are common causes of pericardial effusion.
Physicians recommend bed rest with head elevation at night to lessen the symptoms in these cases.
Potential Symptoms of Fluid Around Your Heart
You might experience:
- shortness of breath
- chest pain,
- fatigue
Other symptoms can include:
- a rapid or irregular heartbeat
- lightheadedness
- or coughing
If the effusion is large, it can compress the heart and interfere with its ability to pump blood effectively. This can cause low blood pressure, shock, or a sudden cardiac arrest.
Seek medical attention if you have any of these symptoms. Pericardial effusions may be treated with drainage, most often through a needle inserted into the pericardium through the neck or an incision in the chest.
The Medical Definition of Pericardial Effusion
Pericardial effusion is an abnormal accumulation of fluid in the space between the layers of the pericardium, the sac-like membrane that surrounds the heart. This can happen due to several different conditions, including infection, inflammation, trauma, or cancer.
Medical Diagnosis for Pericardial effusion
1. An ECG:
An electrocardiogram (ECG) can detect signs of pericardial effusion in people with undiagnosed heart disease or who have just had a heart attack.
Still, it is not sensitive enough to accurately detect pericardial effusion in people without underlying heart disease or who have not had a recent heart attack.
The test can help your doctor determine how much fluid is around your heart and whether it’s causing any problems.
2. Pericardiocentesis
Your doctor may also check for pericardial effusion by using a needle to draw fluid from around your heart. This test, called pericardiocentesis, usually can’t be done if there’s an infection or swelling in your pericardium. So if you have those symptoms, they’ll be treated first.
If your doctor uses a needle, they will put local anesthesia on the skin around the area where they will insert it and ensure that no structures nearby could cause damage if struck. A mild sedative may also be used.
3. X-ray
A doctor may order an X-ray to examine the heart and check for abnormalities. This can be done if an EKG shows abnormal readings or if there are symptoms that suggest pericardial effusion.
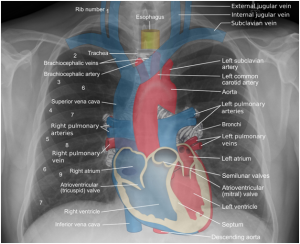
An X-ray picture of the heart used to find fluid around your heart.
Author credit:
By<ahref=”//commons.wikimedia.org/wiki/File:Mikael_H%C3%A4ggstr%C3%B6m_at_pathology_in_2019_(crop).jpg” class=”image”></a><a href=”//commons.wikimedia.org/wiki/File:Mikael_H%C3%A4ggstr%C3%B6m_at_pathology_in_2019_(crop).
X-rays show fluid surrounding the heart and can also show if there are any other problems with the heart.
1. CT or MRI scan
A CT scan or MRI scan can show if there are any problems with your heart’s structure or function (like an enlarged heart).
2. Blood tests
Blood tests can determine if someone has a pericardial effusion because they may reveal an elevated potassium level (hyperkalemia).
Blood tests may also reveal levels of calcium, magnesium, and other electrolytes that can be affected by pericardial effusion. You can also take blood pressure measurements during this appointment to diagnose high blood pressure, among other things.
The level of these minerals should be normal within 24 hours after starting treatment with diuretics to reduce fluid build-up around the heart.
Difference between Fluid Around Your Heart and Fluid Around Your Lungs
Pericardial effusion is the accumulation of fluid around the heart. Excess fluid collects in the pericardium– the heart’s outer covering.
Pericardial effusions can start for many reasons, including infection, inflammation, and obstruction.
Any fluid around your lungs is called pulmonary edema, characterized by excess fluid in the alveoli (the air sacs in your lungs). This can occur as a result of sepsis or congestive heart failure.
3 Ways Pericardial Effusion Happens
Pericardial effusion is a collection of fluid in the heart’s pericardium, the outermost layer. It can occur in three situations:
1. Pulmonary embolus (PE).
This occurs when a blood clot (thrombus) breaks off from a deep vein and travels to the lungs. The PE may then block blood flow from the lung through the superior vena cava to the heart. As a result, fluid builds up in the pericardial sac around the heart and may be visible on an x-ray.
2. Aortic dissection.
This occurs when a tear happens in an artery that carries blood away from your heart to other body parts. Such a tear can lead to bleeding into your pericardium and fluid accumulation within it.
3. Tricuspid valve regurgitation.
This occurs when one or more valves between two chambers of your heart fail to close properly during forceful pumping action by the muscle wall of these chambers.
Treatments for Fluid Around Your Heart
Treatment depends on the cause
- Cancer may need chemotherapy;
- Congestive heart failure may require drugs that relax constricted vessels or procedures like balloon angioplasty;
- Tumors outside the chest cavity may need surgery;
- Non-cancerous conditions often require treatment with corticosteroids, antibiotics, and bed rest.
You can treat pericardial effusions by draining them. Treatment depends on whether they are large or small, how much they have increased, and whether they are causing symptoms.
1. Percutaneous drainage
Small pericardial effusions are drained with a needle inserted through the skin into the sac around your heart (pericardium).
This procedure is called percutaneous drainage and involves putting an IV line in place first before inserting a needle directly into the sac around your heart. It often causes less pain than open surgery.
The procedure may be done under local anesthesia or general anesthesia. The medication used for the injection tends to reduce inflammation and decrease pain.
2. Open surgery
Large pericardial effusions may need to be drained with open surgery to open up your chest cavity and remove any excess fluid from within it. This is called percutaneous nephrostomy or percutaneous thoracoscopy (“through the chest”).
3. Percutaneous cardiopulmonary bypass (PCP)
This procedure uses a mechanical pump to remove fluid from the pericardium and circulate it through the bloodstream. The surgery happens under general anesthesia and takes approximately 30 minutes. It’s considered less invasive than open-heart surgery but has similar risks, including bleeding and infection.
4. Catheter placement
In some cases, catheters placed into the pericardium prevent fluid buildup in the sac surrounding the heart (pericardial space). This procedure is performed under general anesthesia and requires minimal recovery time because no incisions are made during surgery.
5. Antibiotics
Antibiotics treat pericardial effusion if the fluid is infected or contains bacteria. They may also be used for other conditions where the liquid is thick, but the underlying problem is not severe enough to warrant immediate surgery.
Antibiotics are not recommended for patients with pericardial effusions caused by certain viral infections, such as influenza or chicken pox.
6. NSAIDs
NSAIDs (nonsteroidal anti-inflammatory drugs) such as ibuprofen or naproxen can help reduce inflammation and pain from effusion in some patients.
If you have pericardial effusion, your doctor may recommend taking an NSAID daily to reduce the inflammation and pain associated with your condition.
You should not take an NSAID unless your doctor recommends it because it can increase your heart attack or stroke risk.
What are the Prescriptions for Infectious Pericardial Effusion?
If you have infectious pericarditis, your doctor will probably prescribe medications to treat the infection. Here are some of the most common treatments:
1. Antibiotics
Antibiotics help kill germs that cause infection. They may also reduce inflammation and treat complications of pericarditis.
2. Anti-inflammatories
Antiinflammatories reduce pain and swelling by reducing inflammation in the heart’s pericardium (the outer lining).
3. Doxorubicin
Doxorubicin is an antibiotic used to treat certain types of cancer. It’s being tested in people with infectious pericarditis to see if it affects symptoms or how long they’re sick.
4. Inhaled corticosteroids
Inhaled corticosteroids help reduce inflammation in the pericardium by reducing airway edema (swelling of airways).
Causes of Pericardial Effusion in Children
Pericarditis is a diffuse, inflammatory condition of the pericardium. An effusion in the pericardial cavity characterizes it, usually secondary to infection, inflammation, or malignancy.
The outflow may be subacute or chronic.
The leading causes of pericardial effusions include:
1. Infectious pericarditis
This effusion is caused by bacteria or viruses that invade the heart and damage its lining.
Pericarditis can be caused by infection, injury, or malformation of the heart valves and may be accompanied by fever and chills.
2. Myocarditis
Myocarditis occurs when inflammation occurs in the heart muscle, which can cause heart failure if not treated properly.
3. Myocardial infarction
This condition occurs when a heart attack occurs, which damages the heart muscle and causes an acute pericardial effusion due to poor blood supply to the sac and surrounding tissues
4. Compression of the lungs
The most common cause of pericardial effusion is compression of the lungs, usually due to a tumor. The tumor can be benign or malignant and can also be fluid-filled.
5. Blood clots in the pericardium (the sac that surrounds the heart)
Blood clots in the pericardium can cause a small amount of fluid to collect around the heart, leading to a pericardial effusion.
They are rare in children with pericarditis, but if they happen, they typically occur because blood enters through one of two areas:
- One is on top of the heart,
- while another area is on top of a blood vessel between two chambers of the heart (the left atrium and right atrium).
These blood vessels are narrow and have little room for expansion during increased activity, such as coughing or sneezing. This causes a clot to form and block one side of these vessels, increasing pressure against them and eventually leaking into your pericardium.
Clots can also form if a blood vessel and capillaries are injured, such as from blunt trauma or infection with bacteria such as Staphylococcus aureus (Staph).
6. Tumors
Tumors are another possible cause of pericardial effusion in children.
However, these tumors are not always associated with fluid buildup around the heart, although they show up on x-rays as small masses resembling fluid under the skin (radiographic effusions).
7. Congestive heart failure.
This occurs when your heart cannot pump enough blood to meet your body’s needs.
8. Pulmonary embolism.
A blood clot in your lung(s) can travel through a vein into your heart and block blood flow through one or more arteries in your lungs, causing pulmonary hypertension — high blood pressure in your lungs — which can lead to fluid build-up around the heart (pericardial effusion).
Possible Complications of Fluid Around Your Heart
Complications of pericardial effusion can be severe and even life-threatening. The most common ones include:
1. Infection.
The infection can spread to other body parts, including the lungs and brain.
2. Tissue damage.
The tissue surrounding the heart may be damaged by fluid buildup and pressure, which can lead to heart failure or death.
3. Pericardial friction rub.
This occurs when the pressure in the pericardium increases, causing it to rub against the heart wall and cause pain.
Pericardial friction rub may occur if you have a large amount of fluid in your pericardial sac, which can cause it to rub against your heart wall.
This can lead to scarring and thickening of tissue, which can make it more likely that you’ll develop constriction of your heart muscle (myocardial fibrosis).
4. Stroke.
A large pericardial effusion can put pressure on the brain, which can cause a stroke. If you have confusion symptoms or vision loss, seek medical help immediately.
5. Kidney failure.
A pericardial effusion can cause kidney damage and kidney failure if left untreated for too long, especially in people with pre-existing conditions such as diabetes or high blood pressure, making them more susceptible to these complications.
How Common Is Pericardial Effusion?
Pericardial effusions are not as common as other outflows but can be severe.
These outflows can occur along with any kind of heart disease, including congenital heart disease, valvular heart disease, and cardiomyopathy. They can also occur in people who have had a heart attack or had an operation on the heart.
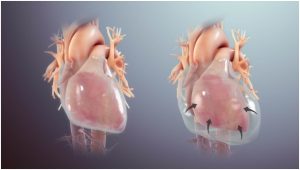
Image alt text: pictorial illustration of a pericardial effusion showing fluid around your heart.
Author credit: By www.scientificanimations.com – <a rel="nofollow" class="external free" href="https://www.scientificanimations.com">https://www.scientificanimations.com</a>, <a href=”https://creativecommons.org/licenses/by-sa/4.0″ title=”Creative Commons Attribution-Share Alike 4.0″>CC BY-SA 4.0</a>, <a href=”https://commons.wikimedia.org/w/index.php?curid=72674453″>Link</a>
Pericardial effusions are more common in older people than younger people and tend to occur more often in men than women. However, there are no apparent differences between them in terms of age or sex.
Still, there is some evidence that women may be less likely to be diagnosed with pericardial effusion than men are.
Is Fluid Around Your Heart an Emergency?
Yes, a large pericardial effusion should be considered an emergency. It can be caused by many conditions, including heart attack, cardiac surgery, or other chest trauma and pericardium trauma. If it is not addressed quickly, it can accumulate fluid in your chest cavity and cause lung and heart problems.
What Could Trigger a Bloody Pericardial Effusion?
A patient with a pericardial effusion has fluid around the surface of their heart. This fluid can be blood or caused by a tear in the heart’s inner lining.
1. Aortic dissection
Aortic dissection is a type of tear in the heart’s inner lining that occurs when a sudden increase in pressure and blood flow within the large arteries supplies blood to your body. It often happens when a blood clot forms between two parts of an artery and they tear apart, causing bleeding into surrounding tissues.
2. Torn muscle
Torn muscle tissue around your heart can also cause bleeding into surrounding tissues if you have an injury that seeps into your pericardium (the membrane surrounding your heart).
What happens if you don’t treat pericardial effusion?
If a pericardial effusion is left untreated, it can increase pressure in the heart, which can damage its muscles and cause it to enlarge. This could eventually lead to a fatal heart attack or stroke.
Visit a doctor if you have any symptoms of pericardial effusion, such as shortness of breath upon exertion, chest pain, or nausea and vomiting.
Aftercare for Pericarditis: What You Need to Know
You’re probably feeling better, your heart is beating again, and you’re back in your routine. But you may still be dealing with some after-effects of acute pericarditis.
Here are some tips on what to expect:
1. Dealing with increased mucus
A week or two after your illness, you might feel like you have a mild cold. That’s because the inflammation of pericarditis causes increased mucus production and congestion in your chest, making you feel congested and uncomfortable.
Make sure to drink plenty of fluids, take frequent rest breaks, and use warm compresses or cooled packs on your chest (on the same side as your heart) to help reduce congestion and other symptoms.
2. Physical activity
In addition to taking it easy, keep up with your usual activities during this time.
However, avoid long periods of intense physical activity, such as running or heavy lifting, because it can make your heart work harder than normal and increase your risk of complications from pericarditis.
Still, light exercises like walking may help build up your strength so that you can get back into shape afterward.
3. Avoid high temperatures and humidity
Also, stay out of high temperatures or humidity as much as possible because both can aggravate symptoms. If you must travel during this period, try to schedule trips.
4. Diet
Follow a strict diet that limits fat and sodium intake, which can lead to fluid retention and swelling in the pericardial sac.
5. Medications
You may need to take medications such as diuretics or beta blockers to help control heart rate or blood pressure.
Last Words on Fluid Around Your Heart
The most common symptom of pericardial effusion is chest pain, but other symptoms may include shortness of breath, fatigue, or an irregular heartbeat.
If left untreated, pericardial effusion can lead to severe complications like cardiac tamponade (a condition in which the heart can’t pump enough blood because of the pressure from the fluid accumulation) or even death.
Treatment can heal pericarditis and allow the heart to recover. Your doctor can help you identify the cause and advise you on the treatment and aftercare for your condition.