Online CPR Certification Blog
How to Stop Venous Bleeding? A Comprehensive Guide
Date: March 12th, 2024
What is Venous Bleeding?
Veins are the blood vessels responsible for bringing deoxygenated blood back to the heart. Venous bleeding is when these vessels get ruptured. As mentioned earlier, the blood is darker, and the flow is steady compared to arterial bleeding.
Explaining the 3 causes of venous bleeding
1.Trauma and Injuries
Venous bleeding occurs as a result of trauma which range from mild to severe. Injuries resulting from accidents like falling at home, or even a vehicle accident, may tear veins. On the contrary, the veins are close to the skin surface while arteries are deep seated inside the body, surrounded by protective tissues such as muscles. External trauma such as cuts and scrapes also pose a danger to them due to their thin skin. It can be simple to cut through a vein, which may result in venous bleeding if the cut goes sufficiently deep.
However, the degree of trauma-induced venous bleeding depends on the type of injury. Sometimes, dark-colored blood might slowly ooze out during a simple scratch or a small wound. The oozing might stop on its own accord or after some minimal intervention. However, a deep cut or a major injury could cause uncontrolled bleeding and require urgent medical intervention. Trauma should also be understood because in some instances some bleeding may not occur yet it can still be heavy venous bleeding.
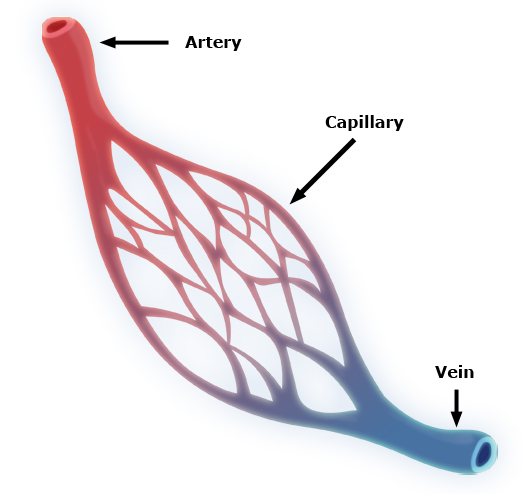
Image alt text: how to stop venous bleeding. An illustration of venous system.
Author credit: By Community Emergency Response Team – http://www.citizencorps.gov/cert/IS317/medops/medops/ic_04_02_0091.htm, Public Domain, https://commons.wikimedia.org/w/index.php?curid=29582984
Finally, trauma-induced venous bleeding can occur anywhere in the body but there are certain parts of the body that are more likely to be affected than others. For example, the legs have extensive venous network which exposes them to trauma and therefore are prone to venous injuries. These measures can be put in place to ensure that protective measures are taken to minimize the chances of such traumas occurring in risky areas or activities.
2.Medical and Surgical Procedures
Even the best medical interventions directed at curing or identifying can accidentally trigger venous bleeding. As surgical procedures involve cutting and handling of tissues within the body. Sometimes, veins are unintentionally nicked or cut by surgeons while operating, a situation that causes bleeding. Even a few extra punctures during non-surgical procedures like needle drawing or IV insertion can cause minor venous bleeding.
The additional concern is post-operative venous bleeding. Occasionally, slow venous bleed may persist even after the closure of the surgical site resulting in hematoma formation in the region. They can be very painful, swollen and give rise to some complications when too big or compress important structures.
It’s crucial for medical professionals to be aware of the potential for venous bleeding during and after procedures. Close monitoring of the surgical or procedural site, ensuring hemostasis (the cessation of bleeding) during the procedure, and informing patients about signs of post-procedural bleeding are all essential steps in the medical realm to prevent and address this cause.
3.Underlying Medical Conditions
Certain medical conditions can predispose individuals to venous bleeding, even in the absence of external trauma or intervention. For example, diseases that affect the integrity of blood vessels, such as vasculitis (inflammation of the blood vessels), can make veins more fragile and prone to rupture. Similarly, conditions that interfere with the body’s clotting mechanism, like hemophilia or certain liver diseases, can lead to prolonged or excessive venous bleeding even from minor injuries.
Chronic venous insufficiency, a condition where the veins don’t work effectively to return blood to the heart, can result in varicose veins. These enlarged, superficial veins are not only cosmetically concerning but are also more vulnerable to injuries and bleeding. A minor bump or scratch can lead to venous bleeding in such cases.
Early diagnosis and management of these underlying conditions are paramount. Regular check-ups, understanding the nature of one’s medical condition, and taking preventive measures can significantly reduce the risk of spontaneous or prolonged venous bleeding associated with these diseases.
Proper management, including medication adjustments and lifestyle changes, can further ensure that the integrity of the venous system is maintained.
The First Line of Treatment: Direct Pressure
When considering how to stop venous bleeding, always remember the golden rule of first aid – Direct Pressure. Here’s how you do it:
- Step 1: Use a clean cloth or sterile bandage to place over the wound.
- Step 2: Apply firm pressure on the wound. Ensure it’s steady but not so strong as to cause harm.
- Step 3: Keep your hands steady and wait. The bleeding should start to decrease or stop completely. If the cloth becomes soaked, do not remove it. Instead, place another cloth over the top and continue the pressure.
Remember that the primary objective is to promote clotting, and by applying pressure, you’re aiding the body’s natural process.
Elevation
Once you’ve got the direct pressure in place, elevating the injury can further help reduce bleeding. If it’s a limb, try and keep it raised above heart level.
This uses gravity to your advantage, reducing the blood flow to the injured area and making it easier to control the bleeding.
Seek Professional Medical Attention
While you might have successfully stopped the bleeding, it’s essential to consult a healthcare professional. They’ll ensure the wound is properly cleaned and, if needed, stitched up. They can also give you a tetanus shot if required.
Commonly Asked Questions
- Is venous bleeding life-threatening? While venous bleeding is generally less dangerous than arterial bleeding, if left unchecked, it can lead to complications, including blood loss. Always treat it with urgency.
- How to differentiate venous bleeding from other types? Venous bleeding is characterized by a steady flow of dark red blood. Arterial blood is brighter red and tends to spurt in time with the heartbeat.
- How long should I apply pressure when trying to stop venous bleeding? You should maintain pressure until the bleeding stops. If after 10-15 minutes of consistent pressure the bleeding hasn’t stopped or slowed, seek emergency medical attention.
- Can I use any cloth to apply pressure? Ideally, you’d want a clean cloth or sterile bandage. However, in emergencies, use whatever you have at hand. It’s crucial to stop the bleeding first.
- Do I always need to see a doctor after venous bleeding? While minor venous bleeds can sometimes be treated at home, it’s always a good idea to consult a doctor, especially if the wound is deep, there’s a risk of infection, or the bleeding was hard to control.
Conclusion
Knowing how to stop venous bleeding is an essential first aid skill that everyone should be equipped with. The first line of treatment is direct pressure, aided by elevation if possible. But always remember, once the immediate situation is under control, seeking professional medical advice is paramount.
Whether you’re a bystander or the one injured, your quick response can make a significant difference in the outcome. Knowledge, prompt action, and a little confidence can go a long way in managing such emergencies. Stay safe and stay informed!