Online CPR Certification Blog
How Do Doctors Determine If Someone Has Heart Disease?
Date: March 9th, 2024
The diagnosis of heart disease is made using a set of tests. First, the doctor will ask about your medical history (your own and your family’s), note any current or recent symptoms, and conduct diagnostic tests such as blood and urine samples and an electrocardiogram. Your doctor may recommend additional testing after reviewing the initial evaluation findings.
It’s important to note that some of these exams don’t require any intrusive procedures, like sticking probes into the patient. Several diagnostic procedures include physically introducing instruments into a patient.
Thankfully, this article covers some methods doctors use to identify a cardiovascular illness. If you suspect you have heart disease, being aware of the symptoms associated with this condition is especially helpful.
Understanding Heart Disease
The term “heart disease” refers to various cardiovascular illnesses that are the leading cause of death in the United States. Some of these diseases include:
- Heart failure
- Congenital heart defects
- Coronary artery disease
Problems with the heart’s rhythm (arrhythmia), like atrial fibrillation
- You may also have
- Heart infections
- Valve disease
- Heart muscle disease or cardiomyopathy
What Are The Symptoms Of Heart Disease?
The signs and symptoms of cardiac disease are often specific to the underlying cause. However, the most common symptoms of heart disease are chest pain or angina caused by inadequate oxygen or arterial nutrient and blood flowing through the heart muscles.
Heartburn or chest pain is the hallmark symptom of angina. Some patients report feeling a pressing or tightness in the area just below their breastbone. Pain radiating from the upper back could spread to the neck, shoulders, arms, or stomach.
You may also have heart disease if you struggle to breathe or tire quickly after a mild effort. In most cases, rest will help these symptoms subside.
Symptoms in women are frequently dissimilar to those in men. Some of the signs that women may experience include: dizziness, shortness of breath, fainting, lightheadedness, jaw discomfort, cold sweats, and a general appearance of weakness.
Also, signs of heart disease may be less evident to women since their symptoms are shared with many different conditions. Anxiety, stress, and the onset of menopause are all variables that are more common in women.
Here are various heart conditions and their symptoms:
Arrhythmias
Many signs and symptoms characterize abnormal cardiac rhythms (also called arrhythmias). You may have a fast or slow heartbeat: It makes your heart feel fluttering, beating too fast, or beating too slowly.
In addition, arrhythmias can lead to:
- Dizziness
- Fainting spells
- Chest pain
- Lightheadedness
Atherosclerosis
With atherosclerosis, fatty plaque deposits cause damage to blood arteries, leading to hardening and stiffness of the vessels. Coronary artery atherosclerosis can cause symptoms, including chest discomfort and shortness of breath. You may also experience the following:
- Coldness and numbness
- Tiredness or weakness in the legs and arms
Congenital heart defect
The term “congenital heart defect” refers to an issue with the heart that is present at birth but originates in the fetal development stage. Pediatricians typically identify the defects at the time of delivery or shortly after.

Image alt text: diagnosis of heart disease. A resuscitation of a person suffering heart attack in progress.
Author credit: By U.S. Navy photo by Photographer's Mate Airman Apprentice Nicholas Garrett. – This image was released by the United States Navy with the ID 040421-N-8090G-001 (next). This tag does not indicate the copyright status of the attached work. A normal copyright tag is still required.
A person may not get a diagnosis until they are an adult, depending on how severe their symptoms are.
Here are some of the symptoms:
- Difficulty breathing
- Slightly bluish skin
- Wearisomely weary
- Inflammation and edema of the limbs
Cardiomyopathy
The damaged heart muscle is called cardiomyopathy. Many symptoms may arise, making a diagnosis of heart disease more challenging. Indicative of these signs are:
- Fatigue
- Bloating
- Fluttering pulse
- Breathing difficulties
- Swollen legs, feet, and ankles
What factors increase your risk of heart disease?
The following are examples of common cardiovascular disease risk factors:
Excess Weight
It’s common knowledge that being overweight or obese raises your risk of developing cardiovascular disease-related diseases, including hypertension and diabetes.
Also, being overweight might cause plaque in your arteries, causing a blockage of blood and other nutrients to your body organs. A heart attack can occur when blockages or damage develop in the arteries supplying blood to the heart. Stroke and vascular dementia are possible outcomes if this happens in the brain’s arteries.
Inactive lifestyle
The accumulation of fatty deposits in the arteries is linked to inactivity. Heart attacks can occur when blockages or damage develop in the arteries that provide blood to the heart. Even worse, the blockage can cause a stroke if it occurs in the brain’s blood vessels.
Fortunately, several cardiovascular disease risk factors can be managed or altered with regular exercise, a significant advantage of this activity. Consistent physical activity can aid in the following:
- Reduce blood pressure
- Reduce the possibility of diabetes.
- Keep a reasonable weight.
- Lessen systemic inflammation
Other benefits include:
- Increases muscle oxygen uptake means the heart doesn’t have to work as hard to supply blood to the body’s muscles.
- It improves HDL cholesterol (the “good”) and aids in managing triglyceride.
- Discourages the production of stress hormones, which might increase cardiovascular strain
- It causes the heart to beat more slowly and the blood pressure to drop, like a beta blocker.
Many studies have indicated that people who engage in regular exercise, even something as simple as walking daily, have a reduced risk of experiencing a sudden and fatal heart attack.
Although exercise offers its own advantages, it is most effective when coupled with a heart-healthy diet. Exercising alone can aid in long-term weight loss. Therefore, a short-term strategy is to decrease calorie intake using a diet while boosting calorie expenditure through activity.
Family history or genetic predisposition to cardiovascular illness
The risk of developing heart disease increases if someone in your family has already had it.
In other words, high blood pressure, high cholesterol, and other risk factors for heart disease tend to cluster in families. When hereditary factors are added to the effects of other risk factors for heart disease, like smoking and poor diet, your risk for the condition can skyrocket.
For this reason, it’s essential to learn about your family’s history of cardiovascular disease to reduce your risk of developing a similar condition.
Diabetes mellitus
Glucose (sugar) is an essential fuel source for the body. Insulin, a hormone produced by the pancreas, facilitates glucose uptake from the blood into the body’s cells. People with diabetes either have insufficient insulin production or impaired insulin use.
Simply put, diabetes occurs when insulin production is inadequate or insulin action is impaired. Since blood glucose levels rise because of diabetes, it’s crucial to discuss diabetes prevention and management strategies with your healthcare provider.
High levels of cholesterol in the blood
Cholesterol is a fatty wax produced in the liver and contained in some meals. Although your liver makes all the cholesterol your body requires, most of us consume too much through our high-cholesterol diets.
Excess cholesterol in the diet can lead to plaque formation in the artery walls, especially those that provide blood to the heart. This causes the arteries to narrow, reducing the amount of blood that can flow through them and reach vital organs like the heart or brain.
High Blood Pressure
One of the leading causes of cardiovascular illness is high blood pressure- a medical disorder that occurs when the blood pressure in the blood vessels, like arteries, is consistently too high. Not taking care of your high blood pressure might damage your heart, kidneys, brain, and other vital organs.
Other Lifestyle Behaviors
One’s way of living can influence the risk of developing cardiovascular disease:
Too much alcohol: Consuming excessive quantities of alcohol is associated with an increase in hypertension and an increased risk of heart disease. It also raises triglyceride levels, a fatty chemical that can raise the risk of cardiovascular disease.
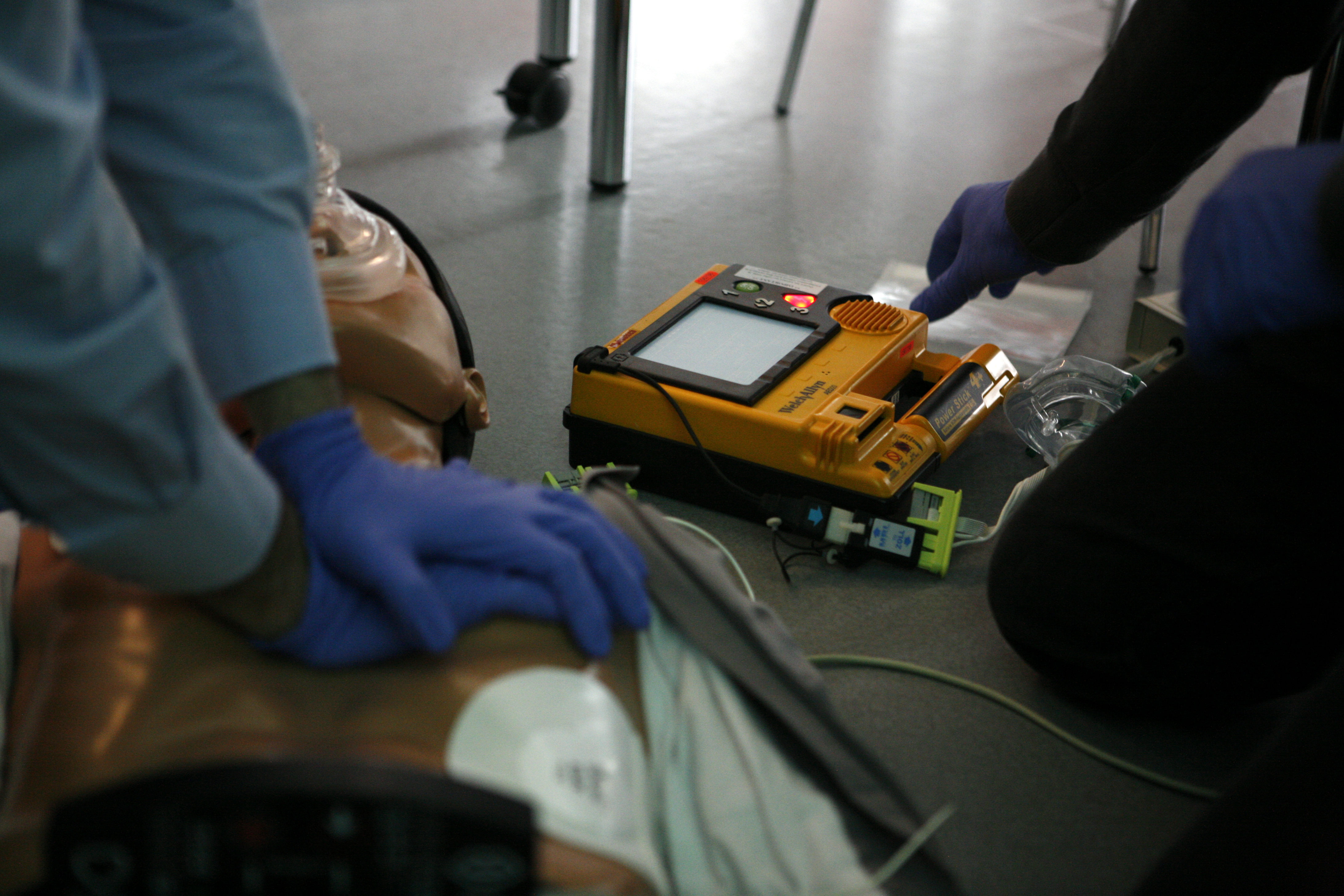
Image alt text: diagnosis of heart disease. A CPR training in progress.
Author credit: By Rama – Own work, CC BY-SA 2.0 fr, https://commons.wikimedia.org/w/index.php?curid=3632271
Using substances containing nicotine and tobacco: There is a correlation between tobacco usage and cardiovascular problems. Heart diseases, including heart attack and atherosclerosis, are made more likely by the harm done to the blood vessels by smoking cigarettes. For instance:
- Smoking raises hypertension
- Carbon monoxide lowers your blood’s oxygen-carrying capacity
- Nonsmokers are also more likely to develop heart disease if they are exposed to secondhand smoke
What to Do If You Think You Have Heart Problems
It’s difficult to tell what’s wrong just by looking at the symptoms. Many diseases and conditions can cause swelling in the lower limbs, exhaustion, and an irregular heartbeat.
It is advisable to find a doctor with whom you can establish a rapport and who can learn about your background and habits. Your doctor’s ability to diagnose your sickness will improve if they know your routine and way of life.
Go in for checks regularly and take your doctor’s recommendations seriously when making positive changes to your daily routine. Consistent medical care is important, but so are lifestyle adjustments.
So, consider the following:
- Quitting smoking
- Staying physically active
- Maintaining a healthy body weight
- Taking heart-healthy diet
- Managing your stress or anxiety
How Do Doctors Determine If Someone Has Heart Disease?
The specific type of cardiac illness being discussed can have a significant impact on how doctors go about making a diagnosis. But of course, most doctors follow a standard procedure to arrive at a diagnosis of heart disease.
Doctors may:
- Do a thorough medical history examination.
- Get a thorough physical examination of the symptoms of heart disease
- Determine which medical procedures will most effectively assist you in concluding the condition
Medical History Examination
The term “medical history examination” is shorthand for an interview where your doctor asks about your health and symptoms to identify any underlying issues.
Your doctor will likely ask you numerous questions about your symptoms, including what sets them off, what relieves them, how long they’ve persisted, when they first appeared, and anything else that might be relevant.
Physical Evaluation
A thorough physical examination may help diagnose various cardiovascular conditions, including arrhythmias.
- Heart valve disease
- Congestive heart failure
- Aortic aneurysm
- Postural orthostatic tachycardia syndrome (POTS)
Clinical Tests with a Focus on Specialty Testing
Many high-tech diagnostic tools have been created for identifying cardiac issues. Although specialist cardiovascular examinations are typically considered the “gold standard” for determining or diagnosis of heart disease, they are most helpful when your medical provider has a strong suspicion that they have the proper diagnosis based on your history and physical exam.
If many tests are necessary, the healthcare provider should base their decision on the results of the first one, as well as any additional information obtained from the patient’s history and physical examination.
If you’re experiencing cardiac issues, your doctor will be able to get to the bottom of things as quickly as possible without putting you in danger of wasting time or money.
The following are some of the specialized testing doctors use in the diagnosis of heart disease:
Electrocardiogram (ECG): An electrocardiogram (ECG) is a recording of the heart’s electrical activity that can provide insight into the heart’s rhythm and significant signals concerning the presence of structural heart disease (such as a previous heart attack or other complications.
Ambulatory Monitoring: An ECG can be recorded for days and weeks with several methods, providing a detailed look at the heart’s rhythm over time. Providers can use these devices to detect and diagnose irregular heartbeats that happen rarely or intermittently.
Tilt test: The doctor can check your BP and heart rate while resting down or standing up using a simple “tilt test.”
This checkup is meant to determine whether or not your reported symptoms, such as fainting or dizziness, are connected to your cardiovascular health. The diagnostic procedure is typically performed during an outpatient visit to an electrophysiology lab.
Heart ultrasound, often known as an echocardiogram: Examining the heart’s motion in real-time is what an echocardiogram does, and it doesn’t require incisions or other invasive procedures. This test, also known as an “echo,” is excellent at spotting heart muscle issues like dilated or restrictive cardiomyopathy, heart valve dysfunction, and the enlargement of cardiac chambers.
The examination takes little time to complete, causes no discomfort to the patient, and does not use radiation. Echocardiography is an excellent screening tool, especially when an individual is at greater risk of heart disease yet shows no symptoms. In addition to its diagnostic value, this test may be repeated over time to track the development of a heart condition.
Stress Testing: Although cardiac stress testing can be helpful in several situations, its primary purpose is to determine whether or not heart disease is causing the heart ischemia that could be blamed for angina and, if so, to determine how severe the problem is.
To determine whether or not the heart muscle is receiving adequate blood flow, a stress test is frequently paired with a thallium scan, which employs a small amount of a radioactive chemical to create an image of the heart. Monitoring the success of anti-anginal medication through stress testing is helpful as well.
Computed Tomography Scan of the Heart: Similar to other types of CT scans, cardiac CTs use computerized X-ray technology to create an organ image. The method can help reveal the calcium deposition around the coronary arteries, thus preventing atherosclerosis before it worsens.
Coronary angiography: Angiograms refer to the images captured during an angiogram procedure. A coronary angiography is performed to view the coronary arteries that provide blood to the heart muscle. It’s the gold standard for identifying coronary artery illness and similar issues with the heart’s vascular system.
The procedure entails inserting a catheter, a long, flexible tube, into a blood artery in your groin. Afterward, the catheter’s tip will reach your coronary arteries and heart.
Arterial narrowing or blockage, the possible cause of your symptoms, might be detected using these photos. Individuals with the heart muscle or valve disorders may also undergo this test to confirm or rule out a diagnosis. After inserting the thin catheter through the coronary arteries, a special dye will be put into them, and X-rays should be taken.
Magnetic resonance imaging: This painless scan produces pictures of the heart and the entire blood vessels using a magnetic field within scanning equipment.
It is effective for detecting issues with heart anatomy and blood supply. Obtaining images from patients whose blood vessels and heart structures are hard to see with angiography is facilitated by this method.
Blood tests: Various blood tests can be performed to rule out alternative causes of heart problems and monitor multiple body levels that can influence the heart. On beginning a new heart medication, blood tests may also be performed.
- Full Blood count (FBC)- This test determines the number of blood cells- red, white, and platelets in the blood.
- Urea and Electrolytes- urea levels assist in monitoring the health of the kidneys, while electrolytes aid in cardiac rhythm stabilization.
- Troponin blood test: When your cardiac muscle is injured, troponin is released into the bloodstream. The troponin level is an immediate and accurate indicator of cardiac muscle injury. Therefore, the test aids in the evaluation of a potential heart attack.
Conclusion
Depending on your symptoms of heart disease, your healthcare provider may conduct a physical exam, blood tests, or other diagnostic methods to look for cardiac or vascular issues. Heart disease can be diagnosed and treated effectively using these tests.
Stroke and heart attack are two of the worst outcomes of cardiovascular illness. Early identification and treatment can lessen the likelihood of problems. If you’re worried, it’s best to consult a medical professional. You’ll learn the signs of heart trouble and the best ways to keep your heart healthy.